Friday 14 October 2016
Even after all these years is male bias still affecting women's chances of surviving heart disease?
It has been known for many years that there are differences in how symptoms of heart disease present in male and female patients, yet it appears that this knowledge is still not translating into better health management practices when assessing and treating women with cardiovascular disease and heart failure.
Excerpts from Australian Catholic University, Mary MacKillop Institute for Health Research, Hidden Hearts: Cardiovascular Risk and Disease in Australian Women, September 2016:
* Executive summary/Key findings
In the absence of a true appreciation of the burden and impact of cardiovascular disease (CVD) among Australian women, coupled with a lack of consistent, Australia-wide data, we compiled this report. Using the best available information, we reveal a number of key figures that should concern all Australians:
The five most common forms of CVD are highly prevalent in Australian women aged 35 years and over with 410,000, 177,000 and 162,000 affected by coronary artery disease (CAD), the form of heart failure (HF) most commonly linked to CAD and atrial fibrillation (AF), respectively.
An additional minimum of 90,000 and 30,000 women are hospitalised due to stroke and peripheral artery disease (PAD), each year. In 2016, 21,000, 14,000, 19,000, 12,000 and 3,000 Australian women will have suffered their first hospital admissions with CAD, HF, AF, stroke and PAD, respectively – see Figure 1.
Tragically, approximately 3,400 Australian women each year will suffer a sudden and fatal cardiac event without ever reaching hospital. Every year, these five conditions provoke a minimum of 260,000 (CAD), 73,000 (HF), 122,000 (AF), 90,000 (stroke) and 30,000 (PAD) hospital admissions among Australian women – see Figure 1.
Even with hospital treatment all forms of CVD are deadly and disabling with one in nine (2,200) women admitted for the first time with CAD dead within 28-days, and more than one third admitted for the first time with HF or stroke dead within 12 months.
The annual estimated cost of hospital care for the most common forms of CVD among Australian women alone is more than $3 billion. Within an ageing population in whom levels of most risk factors are at historically high levels, the burden of CVD among Australian women is set to increase for the foreseeable future.
There is still much to be learned in best preventing and treating CVD in Australian women; particularly in vulnerable individuals/communities.
*
* It is well recognised that the natural history and profile of women with CVD are typically different from their male counterparts.
Current management guidelines reflect a male bias due to the poor representation of women in clinical trials of new therapies.
Women are more likely to display dose-related adverse drug events from CVD pharmacotherapies due to smaller body size, higher body fat, different
metabolism and more kidney dysfunction.
Disparity also exists in cardiac rehabilitation with women failing to attend more often than men in addition to clinicians tending to refer men more frequently.
* Evidence-based management for most forms of CVD are based on clinical trials that have a higher proportion of younger men and/or less complex cases.
* CVD disproportionately affects the Indigenous peoples of Australian and in particular Indigenous women who develop and die from CVD at a much younger age.
* CVD represents an enormous health issue for Australian women. It requires a dedicated response, from the community to governments to minimise already high rates of highly preventable cardiovascular events.
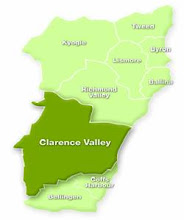
Women living in the Northern Rivers region should note that in 2010-2011, the leading cause of death in the Northern NSW Local Health District was circulatory disease (which includes cardiovascular disease), which was significantly higher than for all NSW - 193/100,000 compared to 167/100,000 according to the December 2015 health fact sheet produced by the NSW North Coast Public Health Unit.
Labels:
health,
North Coast Health,
statistics,
women
Subscribe to:
Post Comments (Atom)



No comments:
Post a Comment